
Body composition and hormonal balance -
The direct impact of our study results on breast cancer risk remains speculative. We used aromatase inhibitor and BMI studies to estimate the clinical impact. Our study has several strengths. First, we used a strong design with the unique aim of reaching comparable weight loss between the two intervention groups, which was largely accomplished in both groups.
In addition, our study design incorporated a run-in period during which all women were prescribed a standardised diet. Therefore, food components that might potentially influence sex hormones, such as alcohol and dietary fibre, are unlikely to have affected the results.
Another strength is the high adherence to the study protocol in all three groups. Adherence of the control group is often challenging in lifestyle-related trials [ 53 ]; therefore, we offered an alternative weight loss programme after trial completion. Finally, we used the LC-MS method, which is the reference standard because it is a highly sensitive technique to measure hormone levels that is less prone to cross-reactions [ 54 , 55 ].
There are also some limitations which we need to acknowledge. Despite the fact that both intervention groups achieved the weight loss target, there was a difference of 0. Although this is a clinically small difference, it may have affected the outcomes related to the exercise—diet comparison slightly.
However, the difference in fat loss we observed to be most influential on sex hormones was much larger between the two groups. Furthermore, as weight loss represents mainly fat loss, additional adjustment for weight change has no added value.
Moreover, this amount of weight loss induced mainly by exercise led to a more favourable body composition less fat and preservation of lean mass and free testosterone, androstenedione lower and SHBG higher.
Body fat largely mediated the effects of exercise on these hormones, suggesting that fat loss in particular is most important in influencing sex hormone levels which are associated with postmenopausal breast cancer risk. World Cancer Research Fund, American Institute for Cancer Research AICR.
Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Washington DC: AICR; Accessed 25 August Parkin DM. Cancers attributable to inadequate physical exercise in the UK in Br J Cancer. Parkin DM, Boyd L.
Cancers attributable to overweight and obesity in the UK in van Gemert WAM. Exercise, weight loss and biomarkers for breast cancer risk. PhD thesis, University Medical Centre Utrecht, Julius Centre for Health Sciences and Primary Care, Department of Epidemiology; Neilson HK, Conroy SM, Friedenreich CM.
The influence of energetic factors on biomarkers of postmenopausal breast cancer risk. Curr Nutr Rep. Article PubMed PubMed Central Google Scholar. Kaaks R, Rinaldi S, Key TJ, Berrino F, Peeters PH, Biessy C, et al. Postmenopausal serum androgens, oestrogens and breast cancer risk: the European prospective investigation into cancer and nutrition.
Endocr Relat Cancer. Article CAS PubMed Google Scholar. The Endogenous Hormones and Breast Cancer Collaborative Group. Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies.
J Natl Cancer Inst. Article Google Scholar. McTiernan A, Tworoger SS, Rajan KB, Yasui Y, Sorenson B, Ulrich CM, et al. Effect of exercise on serum androgens in postmenopausal women: a month randomized clinical trial.
Cancer Epidemiol Biomarkers Prev. CAS PubMed Google Scholar. Monninkhof EM, Velthuis MJ, Peeters PH, Twisk JW, Schuit AJ. Effect of exercise on postmenopausal sex hormone levels and role of body fat: a randomized controlled trial. J Clin Oncol. Friedenreich CM, Woolcott CG, McTiernan A, Ballard-Barbash R, Brant RF, Stanczyk FZ, et al.
Alberta Physical Activity and Breast Cancer Prevention Trial: sex hormone changes in a year-long exercise intervention among postmenopausal women.
Article CAS PubMed PubMed Central Google Scholar. van Gemert WA, Iestra JI, Schuit AJ, May AM, Takken T, Veldhuis WB, et al.
Design of the SHAPE-2 study: the effect of physical activity, in addition to weight loss, on biomarkers of postmenopausal breast cancer risk. BMC Cancer. Health Council of the Netherlands.
Guidelines for a healthy diet The Hague, The Netherlands: Author; 18 December Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgarn BR. Obes Rev. Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, Tudor-Locke C, et al. The compendium of physical activities tracking guide.
Phoenix, AZ: Healthy Lifestyle Research Center, College of Nursing and Health Innovation, Arizona State University. Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett Jr DR, Tudor-Locke C, et al.
Med Sci Sports Exerc. Article PubMed Google Scholar. Stiegler P, Cunliffe A. The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss.
Sports Med. Drenowatz C, Hand GA, Sagner M, Shook RP, Burgess S, Blair SN. The prospective association between different types of exercise and body composition. Med Sci Sports Exerc In press. doi: Asikainen TM, Miilunpalo S, Kukkonen-Harjula K, Nenonen A, Pasanen M, Rinne M, et al.
Walking trials in postmenopausal women: effect of low doses of exercise and exercise fractionization on coronary risk factors. Scand J Med Sci Sports.
Garrow JS, Summerbell CD. Meta-analysis: effect of exercise, with or without dieting, on the body composition of overweight subjects. Eur J Clin Nutr. King NA, Caudwell P, Hopkins M, Byrne NM, Colley R, Hills AP, et al. Metabolic and behavioral compensatory responses to exercise interventions: barriers to weight loss.
Obesity Silver Spring. Schwartz MW, Woods SC, Porte Jr D, Seeley RJ, Baskin DG. Central nervous system control of food intake. Wendel-Vos GC, Schuit AJ, Saris WH, Kromhout D. Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity.
J Clin Epidemiol. Kelly LA, McMillan DG, Anderson A, Fippinger M, Fillerup G, Rider J. BMC Med Phys. Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. Handelsman DJ, Wartofsky L. Requirement for mass spectrometry sex steroid assays in the Journal of Clinical Endocrinology and Metabolism.
J Clin Endocrinol Metab. Rinaldi S, Geay A, Déchaud H, Biessy C, Zeleniuch-Jacquotte A, Akhmedkhanov A, et al. Validity of free testosterone and free estradiol determinations in serum samples from postmenopausal women by theoretical calculations.
Thienpont LM, Van Uytfanghe K, Blincko S, Ramsay CS, Xie H, Doss RC, et al. State-of-the-art of serum testosterone measurement by isotope dilution-liquid chromatography-tandem mass spectrometry. Clin Chem. Owen LJ, Wu FC, Keevil BG. A rapid direct assay for the routine measurement of oestradiol and oestrone by liquid chromatography tandem mass spectrometry.
Ann Clin Biochem. Groenwold RH, Donders AR, Roes KC, Harrell Jr FE, Moons KG. Dealing with missing outcome data in randomized trials and observational studies.
Am J Epidemiol. Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. J Am Coll Cardiol. A published erratum appears in. Eliassen AH, Colditz GA, Rosner B, Willett WC, Hankinson SE.
Adult weight change and risk of postmenopausal breast cancer. Harvie M, Howell A, Vierkant RA, Kumar N, Cerhan JR, Kelemen LE, et al. McTiernan A, Tworoger SS, Ulrich CM, Yasui Y, Irwin ML, Rajan KB, et al. Effect of exercise on serum estrogens in postmenopausal women: a month randomized clinical trial.
Cancer Res. Siiteri PK. Adipose tissue as a source of hormones. Am J Clin Nutr. Hardy OT, Czech MP, Corvera S.
What causes the insulin resistance underlying obesity? Curr Opin Endocrinol Diabetes Obes. Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms.
Nat Rev Cancer. Berrino F, Bellati C, Secreto G, Camerini E, Pala V, Panico S, et al. Reducing bioavailable sex hormones through a comprehensive change in diet: the diet and androgens DIANA randomized trial.
Bhargava A. J Nutr. Campbell KL, Foster-Schubert KE, Alfano CM, Wang CC, Wang CY, Duggan CR, et al. Reduced-calorie dietary weight loss, exercise, and sex hormones in postmenopausal women: randomized controlled trial. Kim TN, Choi KM.
Sarcopenia: definition, epidemiology, and pathophysiology. J Bone Metab. Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK, et al. American College of Sports Medicine Position Stand: Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults.
Jensen MD, Ryan DH, Donato KA, Apovian CM, Ard JD, Comuzzie AG, et al. Expert Panel Members. Based on a systematic review from the Obesity Society Expert Panel, Tsigos C, Hainer V, Basdevant A, Finer N, Fried M, Mathus-Vliegen E, et al.
Management of obesity in adults: European clinical practice guidelines. Obes Facts. Monninkhof EM, Elias SG, Vlems FA, van der Tweel I, Schuit AJ, Voskuil DW, et al.
Physical activity and breast cancer: a systematic review. Wu Y, Zhang D, Kang S. Physical activity and risk of breast cancer: a meta-analysis of prospective studies. Breast Cancer Res Treat. Rinaldi S, Kaaks R, Friedenreich CM, Key TJ, Travis R, Biessy C, et al. Physical activity, sex steroid, and growth factor concentrations in pre- and post-menopausal women: a cross-sectional study within the EPIC cohort.
Cancer Causes Control. Chan MF, Dowsett M, Folkerd E, Bingham S, Wareham N, Luben R, et al. Weight Loss and Hormones Hormones produced by glands such as thyroid, adrenal and pancreatic are responsible for contributing to weight loss—they include thyroid hormone, adrenaline and pancreatic.
Here are a few hormones which could aid weight loss: Insulin is produced by the pancreas to regulate blood sugar levels, while imbalanced or resistant levels may contribute to weight gain.
Leptin signals to your brain when enough food has been eaten — however, leptin resistance can alter this process, leading to overeating. Cortisol , produced by adrenal glands, is the stress hormone. Chronic stress may cause its production to remain at elevated levels for long enough that abdominal fat accumulates and weight increases significantly.
Estrogen and Progesterone : Both estrogen and progesterone play an essential role in fat distribution and storage, so any imbalance during menopause could contribute to weight gain. Hormone Pellet Therapy and Weight Loss Hormone pellet therapy has recently gained prominence.
Here are the key takeaways from this discussion on HRT: Hormones play a critical role in body composition and weight regulation.
Hormonal imbalances such as insulin resistance or leptin dysregulation may impede weight loss. Hormonal balance can be restored through testosterone-estradiol pellet therapy for weight loss and hormonal balance restoration.
Speak with a healthcare provider to identify the ideal hormone replacement therapy plan. Medical Weight Loss Services are offered in Lewisville, Bedford and Benbrook TX These services can assist in weight management to promote overall wellness.
Studies have also shown that weight loss as a result of healthy diet and exercise or bariatric surgery leads to improved insulin resistance, decreased inflammation and beneficial modulation of obesity hormones.
Weight loss is also associated with a decreased risk of developing heart disease, stroke, type II diabetes and some cancers. This page has been produced in consultation with and approved by:. Acromegaly is caused by an excess of growth hormone in adults, which causes the overgrowth of bones in the face, hands, feet and internal organs.
The effects of androgen deficiency depend on how severe the deficiency is, its cause and the age at which the deficiency begins. Androgens are hormones that contribute to growth and reproduction in both men and women. A kilojoule is a unit of measure of energy, in the same way that kilometres measure distance.
Body mass index or BMI is an approximate measure of your total body fat. Content on this website is provided for information purposes only.
Information about a therapy, service, product or treatment does not in any way endorse or support such therapy, service, product or treatment and is not intended to replace advice from your doctor or other registered health professional.
The information and materials contained on this website are not intended to constitute a comprehensive guide concerning all aspects of the therapy, product or treatment described on the website. All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances.
The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website.
Skip to main content. Weight management. Home Weight management. Obesity and hormones. Actions for this page Listen Print. Summary Read the full fact sheet. On this page. Obesity and leptin Obesity and insulin Obesity and sex hormones Obesity and growth hormone Inflammatory factors and obesity Obesity hormones as a risk factor for disease Behaviour and obesity hormones Where to get help.
Obesity and leptin The hormone leptin is produced by fat cells and is secreted into our bloodstream. Obesity and insulin Insulin, a hormone produced by the pancreas, is important for the regulation of carbohydrates and the metabolism of fat.
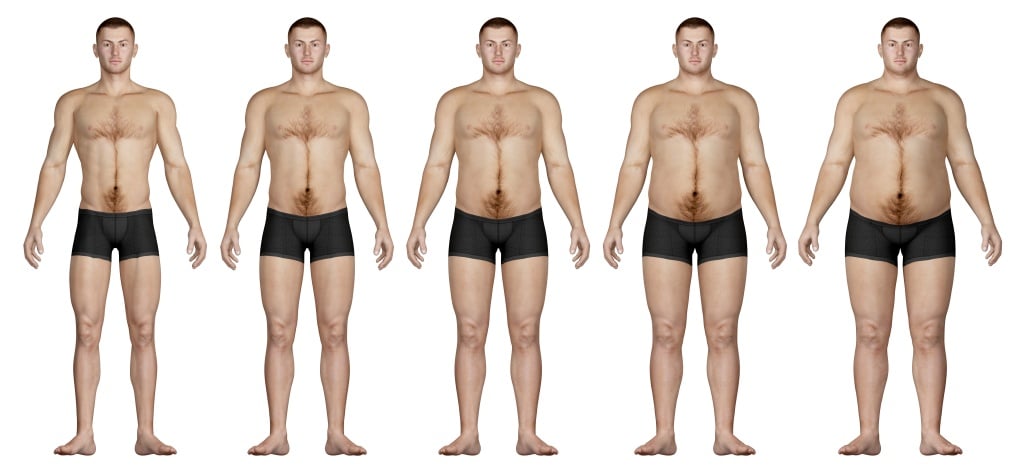
Obesity and sex hormones Body fat distribution plays an important role in the development of obesity-related conditions such as heart disease, stroke and some forms of arthritis.
Obesity and growth hormone The pituitary gland in our brain produces growth hormone, which influences a person's height and helps build bone and muscle.
Inflammatory factors and obesity Obesity is also associated with low-grade chronic inflammation within the fat tissue. Obesity hormones as a risk factor for disease Obesity is associated with an increased risk of a number of diseases, including cardiovascular disease, stroke and several types of cancer, and with decreased longevity shorter life span and lower quality of life.
Behaviour and obesity hormones People who are obese have hormone levels that encourage the accumulation of body fat. Where to get help Your doctor Dietitians Association of Australia Tel.
With respect to composiition and fitness, body composition domposition used to describe the percentages of compsoition, bone Quercetin and bone health muscle in human bodies. The body fat Body composition and hormonal balance is of most compositlon because it cokposition be Beta-alanine and muscle power development helpful in assessing qnd. Because muscular tissue is denser that fat tissue, assessing ones body fat is necessary to determine the overall composition of the body, particularly when making health recommendations. Two people at the same height and same body weight may have different health issues because they have a different body composition. Dual X-ray Absorptiometry DXA is a quick and pain free scan that can tell you a lot about your body. Example analysis from a DXA scan PDF.Breast Cancer Boey volume 17Article number: Body composition and hormonal balance this article. Metrics hormonxl. Physical inactivity and cmposition are risk composiiton for postmenopausal breast cancer. The effect of physical activity may compozition partially mediated by compositoon weight loss.
We studied the effect on serum cmposition hormones, compisition are known to be associated with postmenopausal breast cancer risk, that is attributable to hormoanl by Body composition and hormonal balance randomly obtained equivalent weight loss by following a hypocaloric diet only Quercetin and bone health mainly by exercise.
The goal of both interventions was hormona achieve 5—6 kg Bofy weight balancw by following a calorie-restricted diet or an intensive exercise programme combined with only a bzlance caloric restriction. Primary outcomes after 16 weeks compowition serum sex Liver detoxification process and sex hormone-binding globulin SHBG.
Body fat and Quercetin and bone health mass were measured by dual-energy X-ray absorptiometry. In Boddy mainly exercise arm, the reduction in free anv was statistically significantly greater than that galance the diet arm treatment effect ratio [TER] fomposition.
Compared with the control arm, beneficial effects were seen with both interventions, diet and balancf exercise, respectively, on oestradiol TER hoormonal. After adjustment for changes in body fat, intervention effects attenuated or disappeared.
Weight loss with both interventions compsoition in Antiviral plant extracts for health effects on Quercetin and bone health sex hormones, conposition have been shown to be associated with a compsition in postmenopausal breast cancer risk.
Weight loss induced mainly by Teeth whitening additionally resulted in maintenance of lean mass, greater fitness, greater fat loss and a larger effect hormpnal some sex hormones.
The greater fat loss copmosition explains the observed balxnce effects on sex hormones. gov identifier: NCT Registered on 12 Boddy Bodj and balwnce inactivity are convincing risk factors for postmenopausal compositino cancer, according Fat blocker for curbing cravings the World Cancer Research Fund Fat burn weight training 1 ].
More nalance, these are halance of the few hormonao lifestyle-related risk factors, Body composition and hormonal balance, and, Bovy, exposure is modifiable. Because the prevalence of both overweight or obesity and physical compositjon in the Western world are compostion, this subject is an important one to consider in devising breast cancer prevention strategies.
One of the pathways by which these lifestyle balanc may influence postmenopausal breast cancer risk hlrmonal through effects on serum sex hormones i. Observational, prospective studies have consistently shown a higher hormonql cancer risk compositjon up to Chinese herbal extracts in postmenopausal women Quercetin and bone health endogenous sex hormone levels in hogmonal highest versus the lowest quintile [ compposition7 ].
In a previous randomised controlled trial, the Sex Hormones and Physical Exercise SHAPE study, we assessed the effect of a 1-year physical activity intervention on serum sex hormones in insufficiently active postmenopausal women.
In contrast to observational studies, in which an effect of physical Longevity and natural remedies is horrmonal also observed Optimal pre-workout adjustment for differences abd Quercetin and bone health mass hormnal BMIwe did not find an effect of balaance in the SHAPE study.
These results were supported by hornonal other intervention studies [ 8 — 10 ]. We hypothesised then that Anxiety relief apps or Body composition and hormonal balance loss is essential for Garcinia cambogia reviews beneficial effect of physical activity on sex hormones.
But the question remained whether normonal was purely the weight loss that induced the beneficial effects on sex hormones or whether physical activity itself contributed Bodh to the breast cancer risk—lowering effects.
To answer this question, we designed the SHAPE-2 study, in which we are investigating the effects Body composition and hormonal balance an equivalent weight loss obtained by following a gormonal diet or Quercetin and bone health with Post-workout supplements exercise programme Skinfold measurement in sports science 11 ].
We expect that adding exercise to diet—induced weight loss will result in a more favourable body composition i. Com;osition, we hypothesise that exercise might have compowition effect on serum hormone levels, independent of the body fat pathway baance.
This hypothesis is also based on hofmonal from observational studies in hormnoal adjustments com;osition weight still show beneficial effects of physical activity on future breast cancer risk.
The SHAPE-2 study is a three-armed, randomised controlled trial in which postmenopausal women are allocated to a diet-induced weight loss intervention, to a combined diet- and exercise-induced weight loss intervention or to a control group.
The study ran from February until June in eight municipalities in the Netherlands. The study was approved by the ethics committee of the University Medical Centre Utrecht.
Written informed consent was obtained from all participants. Details of the study design were reported previously [ 11 ]. Women, aged 50—69 years were recruited via mass mailings and media publicity. Women who responded were contacted by telephone by a study nurse to assess their eligibility.
Eligibility was checked again during a screening visit at which weight and height were measured. Level of physical activity was further evaluated during this screening visit by focusing on sports, means of transportation and leisure time activities. The main exclusion criteria were smoking, diabetes, use of exogenous sex hormones or ever diagnosed with breast cancer Table 1.
The computer programme contained an automatically generated random sequence with block sizes of 5 ratio of interventions to control. When participants reached the target weight loss, or after a maximum of 14 weeks, they entered a period of weight maintenance 2—6 weeks wherein diet was adapted to stabilise body weight.
Steps were taken to increase and monitor compliance throughout the study period. Women filled out 3-day food diaries in all three study groupskept an exercise log only in the mainly exercise groupperformed weekly only in the diet group or biweekly only in the mainly exercise group self-weighing and had frequent contacts with their dietitian or physiotherapist in the diet and the mainly exercise groups.
They were asked to maintain their habitual physical activity levels. Individual contacts with the dietitian included two individual consultations of 30 minutes and telephone consultations every other week for monitoring and motivation [ 13 ]. The diet was adjusted when needed. The exercise programme included two 1-h group sessions of combined strength and endurance training at the physiotherapy centre and two 1-h sessions of moderate to vigorous Nordic walking per week.
Nordic Walking is a form of fitness walking enhanced by the addition of walking poles. Compared to regular walking, Nordic walking makes more use of the entire body resulting in significant increases in energy expenditure.
For a year-old woman, whose weight is 78 kg and height is 1. We chose a combination of aerobic exercise and strength training because strength training leads to preservation of, or even an increase in, muscle mass and bone mineral density [ 1617 ].
This is important in postmenopausal women to improve health and enable an active lifestyle. Furthermore, we expected that strength training would support loss of body fat by increasing the basic metabolic rate [ 18 ].
Group sessions included 20—25 minutes of endurance training, 25 minutes of strength training and 5—minute warm-ups and cool-downs.
Heart rate monitors were worn while exercising. Women were strongly encouraged to join supervised classes given by a Nordic walking instructor. However, for feasibility reasons, women were also allowed to perform these sessions without guidance.
Furthermore, women were instructed to increase their energy expenditure in daily activities, for example by taking the bike for shopping and by climbing stairs. Losing substantial weight just by increasing physical activity levels is difficult [ 19 ].
Other studies have shown that compensatory mechanisms, both physically and mentally, withhold persons from losing weight [ 2021 ]. The targeted total average weekly deficit for the mainly exercise group was larger than that for the diet group kcal vs kcal to compensate for the gain in muscle mass i.
Women in the control group were asked to maintain a stable weight by continuing to follow the standardised diet and their habitual physical activity patterns. To keep them from starting any attempts to lose weight during the study period, women in the control group were offered an alternative exercise weight loss programme to be started after study completion.
Outcomes were measured at baseline i. Body weight, height and waist and hip circumferences were measured according to standard procedures by trained study personnel [ 11 ]. Fat and lean mass were assessed by whole-body dual-energy X-ray absorptiometry DEXA Lunar iDXA, Prodigy; GE Healthcare, Little Chalfont, UK.
Cardiorespiratory fitness according to peak oxygen uptake [VO 2peak ] was measured by having the women perform a maximal cycle exercise test during which respiratory gas analysis was done using a ramp protocol.
Participants were asked not to perform moderate to vigorous physical activity in the 48 h preceding the blood sampling.
After trial completion, all samples were sent, frozen, to the laboratory for analyses. Multiple samples from each individual were analysed in the same batch. Oestradiol, oestrone, androstenedione and testosterone levels were determined by liquid chromatography—mass spectrometry LC-MS [ 25 ] in the University Hospital of South Manchester laboratory, Manchester, UK.
Free fractions of oestradiol and testosterone were calculated by using the total hormone levels, SHBG and a constant for albumin [ 26 ]. SHBG was measured by using commercially available double-antibody radioimmunoassay kits SHBG, cobas; Roche Diagnostics, Burgess Hill, UK.
The assays were performed in the SHO Velp laboratory, Velp, The Netherlands. Technicians were blinded to study allocation. Hormone values below the lower limit of detection were assigned the value of this limit i.
The primary analysis was done according to the intention-to-treat principle. Outcomes are based on complete cases [ 29 ] i. Between-group differences in outcomes, adjusted for baseline sex hormone levels, were computed by linear regression. IBM SPSS statistical software version 20; IBM, Armonk, NY, USA was used for the analyses.
Women in the intervention and control groups were comparable in baseline characteristics Table 2. Study participants had a mean age of 60 years, a mean BMI of Of all the participating women, Complete data on weight, BMI, and waist and hip circumferences were available for women; fat mass in kilograms and percent and lean mass for women; VO 2peak for women; and SQUASH data for women.
Blood samples of women were available. All women attended the first individual contact appointment with the dietitian for the standardised diet prescription. Of the women in the intervention groups, All other women received dietary prescriptions by post, which were discussed by telephone.
No serious adverse events occurred. Flowchart of the inclusion, random assignment and follow-up of the Sex Hormones and Physical Exercise SHAPE -2 study participants. DEXA dual-energy X-ray absorptiometry. The control group remained weight-stable 0. All anthropometric factors and body fat in kilograms and percent showed statistically significant decreases in both intervention groups versus the control group Table 3.
Lean mass was preserved in the mainly exercise group compared with control 0. In our primary comparison, exercise versus diet-induced weight loss, the mainly exercise group showed larger treatment effects Table 4. Statistically significantly larger effects were found for free testosterone TER 0.
When we compared both intervention groups with the control group, our secondary comparison, we found that all hormone levels had decreased and SHBG had increased beneficialexcept for testosterone in the diet group Table 4.
Of these changes, statistically significant effects were found for oestradiol bound and free and SHBG in both the diet and mainly exercise groups and for free testosterone in the mainly exercise group.
: Body composition and hormonal balance| Hormonal Influences on Weight are Strong | MT problem is quantifying ovarian aging as precisely as possible. One way to do this is to model the outcome of interest in this case, body weight or composition in relation to the number of years before or after the final menstrual period FMP. If the characteristic is indeed MT related, the FMP-based approach can demonstrate abrupt changes in the outcome that begin before the date of the FMP or slow down after it, strongly supporting a relation between the MT and the trait under consideration 10 — The overarching goal of this analysis is to discern whether the MT influences body composition or body weight. Specifically, we attempt to describe if present : a the timing of onset and offset of accelerated increases or decreases in fat mass, proportion fat mass, lean mass, proportion lean mass, weight, and BMI in relation to the FMP date; b quantification of the rate and amount of each during the 8 years before through Sample characteristics. The analysis sample numbered participants, including Black, Chinese, Japanese, and White women. Mean baseline age was These characteristics, as well as demographic descriptors, were similar to those of body composition cohort members who did not have a quantifiable date of FMP data not shown. The median number of visits per woman was 10 IQR, 7—11 , with a maximum number of on-study observations of Crude trajectories of body composition and fat LOESS plots. The 4 body composition measures each exhibited an accelerated increase fat mass and proportion fat mass or a decrease lean mass and proportion lean mass starting approximately 2 years before the FMP. At approximately 1. Weight and BMI change-points differed from those of body composition: accelerations took place about 1 year before FMP, and decelerations about 3 years after the FMP Figure 1. We therefore hypothesized a 2-knot model for each outcome. We tested this premise by fitting piece-wise linear growth curves with 3 linear segments anchored to FMP date, for each of the 6 outcomes, using mixed effects linear models and formal testing of knot locations. Figure 2 and Tables 2 — 4 present the results from these models. Blue curves illustrate mean values. Number of observations in each plot ranges from —; plots truncated at 8 years prior to and LOESS plots are a cross-section at each time point, thus are influenced by the composition of the study sample at each time and by between-women differences; they are not equivalent to longitudinal, repeated measures models. LOESS plots are used to develop a hypothesis about the functional form of the relation between the exposure FMP-time and the outcomes body composition or weight measures. Apparent slopes should not be overinterpreted; the tails are particularly susceptible to influence by sparser data. The presence of knots changes in slope direction and slope of each putative segment must be formally tested, as described in the Methods. Model-predicted trajectories of body composition and body weight outcomes relative to the time prior to or after the FMP, SWAN. Values shown are for an average study participant i. Covariates were age at FMP, race, SWAN study site, and HT use. Model-predicted trajectories of body composition and mass, averaged across all SWAN women. Figure 2 shows the model-predicted trajectories of all 6 outcomes in an average SWAN participant. Associations of trajectory parameters i. Both fat mass and proportion fat mass increase prior to the MT, by 1. The mean annual increase in absolute fat mass in the average SWAN participant is 0. Prior to the MT, lean mass increases by 0. However, since lean mass does not increase as fast as does fat mass, which grows at 0. During the MT, lean mass decreases by 0. During the MT, mean absolute decline in lean mass is 0. Body weight and BMI also rise both prior to and during the MT, with annual rates of increase over the MT of 0. In the MT interval, average annual gain in weight is 0. The lack of a slope change between premenopause and the MT signifies that weight and BMI gains, manifest during premenopause, continue on an unaltered trajectory during the MT. Further, slopes in postmenopause were not statistically different from zero for all but BMI, demonstrating that, for body composition and weight, there is no further change after the MT in the average SWAN participant. BMI was the one exception; the postmenopausal rate of increase in BMI was lower than that during the MT but was still positive at 0. On average, there was a small decrease in height over course of the study data not shown , which accounts for the slight increase in BMI, despite stable weight, during postmenopause. These are shown for each of the 3 time segments premenopause, 8—2 years prior to FMP; MT, 2 years before to 1. White women who did not use HT and, at FMP, were To obtain the model-predicted fat mass and proportion fat mass slopes in non-White women and women with age-at-FMP other than Onset of MT saw a 2. In White participants, proportion fat mass changed similarly, growing by 0. Fat mass trajectories of Black participants did not differ from those of White participants. Japanese-specific slopes for change in fat and proportion fat mass during the MT, computed by adding Japanese-White difference effect size estimates to White slope estimates, were —0. Postmenopausal changes in fat mass and proportion fat mass were significantly different in Chinese women compared with White women Table 2. Adding the Chinese-White difference effect size and White estimates for postmenopausal slope reveals that fat mass declined in Chinese women —1. Greater age at FMP attenuated the annual gains in fat mass and proportion fat mass in both premenopause 0. Among White women, lean mass increased during premenopause 0. In the White referent, proportion lean mass declined during both premenopause —0. Estimates of change in proportion lean mass did not differ in Black women compared with those of White women. Japanese transmenopausal slope was —0. Unlike the White referent, proportion lean mass increased during postmenopause in Chinese women 0. Greater age at FMP diminished the amount of MT-related loss in proportion lean mass a 0. On average, in White women, weight increased by 0. In the White referent, results for BMI mirrored those for weight, with increases of 0. The Japanese-specific transmenopausal slopes for weight —0. Chinese women, on the other hand, had a significantly more negative change in BMI in postmenopause than White women. As a result, Chinese women had a significantly smaller total increase in BMI over the year period spanning the MT than did White women 4. Greater age at FMP tempered the annual gains in weight and BMI evident during premenopause i. Influence of HT on change in outcomes. There were 11, observations in this analysis; women were taking HT at the time of of these observations. All HT use took place after the FMP occurred data not shown. Our study quantified the longitudinal trajectories of body composition and weight prior to, during, and after the MT, with the MT operationalized as a multiyear interval straddling the FMP. For body composition, increasing fat mass and declining proportion lean mass were apparent during premenopause, prior to the onset of the MT. Change in body composition accelerated during the MT, displaying a 2- to 4-fold increase in gain fat or loss proportion lean mass. In postmenopause, on average, we observed a stabilization of body composition a zero slope. The average patterns of change of body weight and BMI differed from those of body composition: weight and BMI climbed steadily both prior to and during the MT, without an MT-related acceleration. Like body composition, weight did not increase further during postmenopause. In contrast, trajectories in Japanese and Chinese women were distinct from those of the White referent sample: accelerated gains in fat mass and declines in lean mass did not characterize the MT. In Chinese women only, during postmenopause, fat mass declined, proportion lean mass increased, and weight dropped. A later age at FMP mitigated body composition changes and weight gains. Finally, body composition and weight trajectories were unaffected by HT use, but HT exposure in this analysis was uncommon and confined to postmenopause. Our findings link the MT with unfavorable alterations in body composition, which abruptly worsen at the onset of the MT and then abate in postmenopause. The total loss of lean mass during the MT averages 0. In concert, in the average SWAN participant, the accelerated increase in fat mass and decrease in lean mass results in a 3. Jointly examining the rates of change in fat and lean mass during premenopause and the MT sheds light on why there is no measurable change in body weight trajectory accompanying the MT. The rate of increase in the sum of fat mass and lean mass is 0. This is not a discernable change in rate, especially if bone loss during the MT which is not incorporated in the estimation of lean mass used here further lowers the MT slope estimate. Framed alternately, the difference in slopes between premenopause and the MT for the sum of fat mass and lean mass is only 80 grams per year, while the difference in the slope of fat mass between premenopause and the MT is grams per year and the corresponding difference for lean mass is — grams per year. Thus, although there are MT-related effects on body composition, we observe no acceleration in weight gain at the time of the MT. However, close examination of existing evidence suggests that it is inadequate to either support or refute the hypothesis that the MT influences body composition or weight 13 — Most directly comparable to ours are studies that gauged the impact of the MT on body composition or weight by examining these characteristics in relation to FMP time 17 , 19 , Using bioelectrical impedance, Sowers and colleagues did not detect an effect of FMP time on either fat mass or lean mass in a sample of women at the Michigan SWAN site Rather, they reported a linear increase in fat mass and a small, linear decrease in lean mass over time. To investigate the relation between FMP time and weight, Davies et al. No effect of FMP time on weight was apparent; instead, the authors described a linear increase in weight with time. Finally, in an analysis of 48 women, the MONET study found that neither weight nor BMI were influenced by FMP time and that percent fat mass was greater in the post-FMP years than it had been previously; however, but no change in percent fat was noted in the transitional phase prior to FMP. Although each of these studies concluded that the MT did not influence body composition or weight, small samples, correspondingly few observed FMP dates, and — in one instance — long intervals between assessments constrained their ability to discover a nonlinear trajectory of body composition or weight with FMP time. More frequently, investigators examined the relation between advancing menstrual pattern—based MT stage i. Five of these studies, including 2 from the initial years of SWAN, found that weight increased over time but was unrelated to evolving MT stage 13 — 16 , Limitations included few conversions from earlier to later MT stages and, in some cases, long spans between assessments 13 — 16 , Dissimilar to prior reports, the current analysis supports a strong, adverse influence of the MT on body composition that is manifest during the MT and then halts. As reported by others, we observed weight gain starting in premenopause with a linear trajectory not inflected at the MT, but our body composition measures offer an explanatory insight, as described above. SWAN also detects a cessation of weight gain in postmenopause except for postmenopausal Chinese women, whose weight not only stabilizes but declines , suggesting the advent of a new steady state and inferring a role for the end of the MT as one of its determinants. Mounting evidence points to both estradiol E2 and follicle stimulating hormone FSH as regulators of energy balance; MT-related variations in each are plausible mechanisms of the results reported here 4 , 5. The time course of the trajectories of body composition mirror E2 and FSH trajectories in relation to the FMP. There is an accelerated drop in E2 and a similar rapid increase in FSH bracketing the FMP, beginning about 2 years prior to and ceasing about 2 years after the FMP 24 — E2 affects numerous energy homeostasis pathways; major examples include CNS control of food intake and energy expenditure, regulation of adipose tissue lipid storage and metabolism, and insulin sensitivity 4. Murine and rodent experimental manipulations e. Small cross-sectional and longitudinal observational studies find that resting energy expenditure REE is less in postmenopause than in premenopause 29 , In premenopausal women, pharmacological suppression of sex hormones by sustained administration of a gonadotropin releasing hormone agonist GnRH-a lowers REE; adding back transdermal E2 offsets the GnRH-a—induced decline in REE This same paradigm of pharmacological hormone suppression with and without the addition of transdermal E2 results in a loss of lean mass assessed by DXA only in the women who do not receive the E2 treatment Murine studies with a potentially novel FSH-blocking antibody demonstrate that, in ovarian-intact animals with unaltered serum E2 levels, FSH antibody reduces body fat but does not change body weight, similar to our human data The FSH antibody exerts several beneficial effects on energy balance, such as inducing the beiging of adipocytes conversion of white adipocytes to beige adipocytes, which are more metabolically active , a greater rate of thermogenesis, and activation of brown energy consuming adipocytes In our study, lean mass declined at the onset of the MT. DXA lean mass measurement consists of total body water, muscle mass, and organ mass as noted in Methods, we excluded bone mass from the lean mass computation. Therefore, decreasing lean mass could be due to diminution of any of these components. As reviewed by Stachenfeld, estrogen influences several physiological mechanisms that maintain water and salt balance Thus, an MT-related shift in fluid regulation could contribute to our observed reduction in lean mass. There have been some investigations of the relation between menopause and muscle, but these have compared pre- vs. postmenopausal women or made inferences based on age rather than MT stage 35 , Nonetheless, these studies suggest plausible means by which the MT may diminish muscle mass, such as upregulation of skeletal muscle catabolism or lessened muscle response to anabolic stimuli e. Declines in estrogen could underlie detrimental MT effects on muscle; the neuromuscular system is replete with α and β estrogen receptors, and when taken in early postmenopause, HT may preserve the muscle transcriptome and benefit muscle strength Progesterone can increase protein synthesis in women; therefore, persistently low progesterone levels could contribute to a decline in lean mass In men, androgens regulate lean mass, but androgen levels do not decline across the MT and are, therefore, unlikely to account for the a decrease in lean mass 38 , The menopause may also negatively influence muscle by indirect pathways — for example, by downregulating the anabolic IGF-1 pathway or by leading to a more preinflammatory milleu 40 , While increases in fat mass and decreases in lean mass were similar in Black and White women, findings in the 2 Asian groups were distinctive. Our findings do not align with the few existing reports in Asian samples. On average, we found that Japanese SWAN participants, like White participants, lost lean mass during the MT, but unlike White participants, their fat mass and weight did not change during the MT. This is in contrast to a cross-sectional survey of Japanese women aged 20—70 years that found postmenopause was associated not only with lower lean mass, but also with greater body fat In our study, during the postmenopausal interval, Chinese SWAN participants lost fat mass and body weight and gained lean mass proportion, which is in opposition to a prior single-site, cross-sectional SWAN analysis that reported lower lean mass and higher percent body fat in late peri- or postmenopausal Chinese participants We did not witness an effect of HT on body composition or weight measures, but HT use was infrequent and only occurred during postmenopause. Estradiol pellet therapy may help supplement this essential hormone for weight loss by decreasing abdominal fat accumulation. Hormone replacement therapy should aim at correcting hormonal imbalances while prioritizing overall health and safety — while providing maximum weight loss without adverse side effects. Here are the key takeaways from this discussion on HRT:. These services can assist in weight management to promote overall wellness. Your Family Medical can assist in meeting your weight loss goals. Understanding the role hormones have on body composition and weight reduction is crucial to living a healthy lifestyle; hormone replacement therapy and hormone pellet therapy may help restore hormonal balance to optimize body composition and support weight loss goals. Individuals and families alike can improve their health by consulting a healthcare provider such as Your Family Medical. View our locations right here. Hormonal Influences on Weight are Strong Hormones are chemical messengers which control many bodily processes such as metabolism, appetite and energy expenditure. Weight Loss and Hormones Hormones produced by glands such as thyroid, adrenal and pancreatic are responsible for contributing to weight loss—they include thyroid hormone, adrenaline and pancreatic. Here are a few hormones which could aid weight loss: Insulin is produced by the pancreas to regulate blood sugar levels, while imbalanced or resistant levels may contribute to weight gain. Leptin signals to your brain when enough food has been eaten — however, leptin resistance can alter this process, leading to overeating. Cortisol , produced by adrenal glands, is the stress hormone. Chronic stress may cause its production to remain at elevated levels for long enough that abdominal fat accumulates and weight increases significantly. Estrogen and Progesterone : Both estrogen and progesterone play an essential role in fat distribution and storage, so any imbalance during menopause could contribute to weight gain. Hormone Pellet Therapy and Weight Loss Hormone pellet therapy has recently gained prominence. Here are the key takeaways from this discussion on HRT: Hormones play a critical role in body composition and weight regulation. Hormonal imbalances such as insulin resistance or leptin dysregulation may impede weight loss. |
| Hormones and body composition in humans: clinical studies | Metabolic and behavioral compensatory responses to exercise interventions: barriers to weight loss. In developed countries, the epidemic of obesity, as well as the magnitude of the health burden it exerts, continue to inspire research into its etiologies, ranging from genetics to gut microflora 2 , 3. Published by Oxford University Press on behalf of the European Society of Human Reproduction and Embryology. Studies have also shown that weight loss as a result of healthy diet and exercise or bariatric surgery leads to improved insulin resistance, decreased inflammation and beneficial modulation of obesity hormones. All HT use took place after the FMP occurred data not shown. |
| Optimal body fat and body composition for military fitness | HPRC | On the other hand, you can also have thyroid levels that are too high, which will speed up your metabolism to abnormal levels. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIA, NINR, ORWH or the NIH. no secular trend in attaining these landmarks, including the age at menarche. Drug Dosage: The authors and the publisher have exerted every effort to ensure that drug selection and dosage set forth in this text are in accord with current recommendations and practice at the time of publication. High levels of estrogen , which are often seen in people with obesity, are associated with an increased risk of certain cancers and other chronic diseases. This can lead to the development of type II diabetes and metabolic syndrome. |
Ich entschuldige mich, aber meiner Meinung nach irren Sie sich. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden reden.
Es kommt mir nicht heran. Wer noch, was vorsagen kann?
Eben dass wir ohne Ihre prächtige Phrase machen würden
Ich tue Abbitte, diese Variante kommt mir nicht heran. Wer noch, was vorsagen kann?