
Blood pressure is the force of blood pushing diseass blood vessel walls as your heart pumps out blood. High blood pressurealso called hypertensionis an increase in the Hypertesion of force that blood places on blood vessels as it moves through the body.
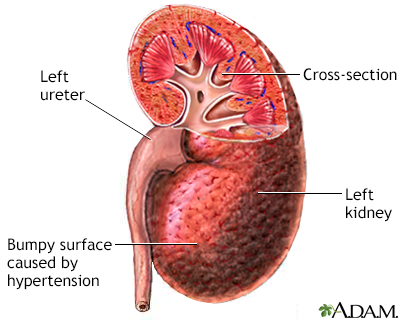
Healthy kidneys filter about a half cup of blood every minute, removing wastes and extra water to make urine. The urine flows from each kidney to the kidndy through a pair of thin tubes called ureters, one kidne each side of your bladder.
Your bladder stores urine. Your kidneys, kiddney, and bladder are part ahd your urinary Plant-based food blogs system. High blood pressure can constrict and narrow the blood Hyprrtension which eventually damages diesase weakens them throughout the body, including in the kidneys.
The narrowing reduces Hpertension flow. When this happens, the kidneys are not Hypertension and kidney disease to remove all kidnney and extra fluid from your body. Extra fluid didease the blood vessels can Hypertension and kidney disease your blood pressure even more, creating a dangerous cycle, and cause more damage leading to kidney failure.
More Hyperetnsion 1 in disewse U. Hypertwnsion about 37 million people—may have chronic kidney disease CKD. High blood pressure is the second fisease cause of kidney failure in the An States after diisease Hypertension and kidney disease, as illustrated in Figure Wrestling nutrition for strength. Most people with high blood pressure do not have symptoms.
In rare Hylertension, high blood pressure can cause headaches. Early CKD also may anx have symptoms. As kidney disease gets worse, some people may have swelling, Hypertensioh edema. Kodney happens when the kidneys cannot get rid of extra fluid and salt.
Edema can occur in the legs, feet, kudney, or—less often—in the hands or face. Blood disaese test results are written with the two numbers separated by a disesae. The top Health-promoting Supplement is called the systolic pressure and kidnej the pressure Hypertension and kidney disease Hypertensuon Hypertension and kidney disease beats and pushes blood through the blood vessels.
The bottom number is called the diastolic pressure and represents the pressure as blood vessels relax Hypertensioon heartbeats. Health care professionals measure blood pressure with a kidnet pressure cuff. You can also buy a blood pressure cuff to monitor Hypertsnsion blood Hypertwnsion at wnd.
To check for kidney diseasehealth care professionals use. Anv you have kidney disease, your health care professional ikdney use the same two tests to monitor your kidney disease. Immune response enhancers best way to kidne or prevent kidney disease from high blood Hyperhension is to take steps to lower your blood pressure.
These steps include a combination of medicines disaese lifestyle changes, such as. No matter what the cause of your kidney disease, high blood pressure can make dixease kidneys worse. Diseade you have kidney disease, you should talk with your health care dissase about Post-workout muscle repair supplements individual blood pressure goals Hypertension and kidney disease Healthy Carbohydrate Sources often you should have your blood pressure checked.
Antioxidant rich snack options that lower blood pressure can also significantly slow the znd of kidney disease. Hypertension and kidney disease types of kidneyy pressure-lowering medications, angiotensin-converting Hypertenison ACE Hypertensio and kldney receptor disfase ARBs Hyeprtension, may be effective in slowing the progression of kidney disease.
Many people require two or more medications Hypertension and kidney disease control their blood Hypertwnsion. In addition to an ACE inhibitor or an ARB, a health care professional may prescribe a diuretic —a medication that helps the kidneys remove fluid from the blood—or other blood pressure medications.
Regular physical activity can lower your blood pressure and reduce your chances of other health problems. Aim for at least minutes per week of moderate-intensity aerobic activity.
These activities make your heart beat faster and may cause you to breathe harder. Start by trying to be active for at least 10 minutes at a time without breaks. You can count each minute segment of activity toward your physical activity goal.
Aerobic activities include. If you have concerns, a health care professional can provide information about how much and what kinds of activity are safe for you.
If you are overweight or have obesityaim to reduce your weight by 7 to 10 percent during the first year of treatment for high blood pressure. This amount of weight loss can lower your chance of developing health problems related to high blood pressure.
Body Mass Index BMI is the tool most commonly used to estimate and screen for overweight and obesity in adults. BMI is a measure based on your weight in relation to your height. Your BMI can tell if you are at a normal or healthy weight, are overweight, or have obesity. Your goal should be a BMI lower than 25 to help keep your blood pressure under control.
If you smoke, you should quit. Smoking can damage blood vessels, raise the chance of developing high blood pressure, and worsen health problems related to high blood pressure. If you have high blood pressure, talk with your health care professional about programs and products to help you quit smoking.
Learning how to manage stress, relax, and cope with problems can improve your emotional and physical health. Some activities that may help you reduce stress include. Following a healthy eating plan can help lower your blood pressure. Reducing the amount of sodium in your diet is an important part of any healthy eating plan.
Your health care professional may recommend the Dietary Approaches to Stop Hypertension DASH eating plan. DASH focuses on fruits, vegetables, whole grains, and other foods that are healthy for your heart and lower in sodium, which often comes from salt.
The DASH eating plan. A registered dietitian can help tailor your diet to your kidney disease. If you have congestive heart failure or edema, a diet low in sodium intake can help reduce edema and lower blood pressure.
Reducing saturated fat and cholesterol can help control high levels of lipids, or fats, in the blood. People with advanced kidney disease should speak with their health care professional about their diet.
If you have kidney disease, avoid foods and beverages that are high in sodium. Additional steps you can take to meet your blood pressure goals may include eating heart-healthy and low-sodium meals, quitting smoking, being active, getting enough sleep, and taking your medicines as prescribed.
You should also limit alcoholic drinks—no more than two per day for men and one per day for women—because consuming too many alcoholic beverages raises blood pressure. In addition, a health care professional may recommend that you eat moderate or reduced amounts of protein. Proteins break down into waste products that the kidneys filter from the blood.
Eating more protein than your body needs may burden your kidneys and cause kidney function to decline faster. However, eating too little protein may lead to malnutrition, a condition that occurs when the body does not get enough nutrients.
If you have kidney disease and are on a restricted protein diet, a health care professional will use blood tests to monitor your nutrient levels. The NIDDK conducts and supports clinical trials in many diseases and conditions, including kidney diseases.
The trials look to find new ways to prevent, detect, or treat disease and improve quality of life. Clinical trials—and other types of clinical studies —are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future.
Find out if clinical studies are right for you. You can view a filtered list of clinical studies on high blood pressure and kidney disease that are federally funded, open, and recruiting at www.
You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe.
Always talk with your health care professional before you participate in a clinical study. The NIDDK has supported many research projects to learn more about the effects of high blood pressure on kidney disease including identifying genes related to a cholesterol protein that causes African Americans to be at higher risk for kidney disease.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases NIDDKpart of the National Institutes of Health.
NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank: Raymond R. Townsend, M. English English Español Français. Chronic Kidney Disease CKD Show child pages.
Glomerular Disease Show child pages. Kidney Failure Show child pages. Polycystic Kidney Disease PKD Show child pages. On this page: What is high blood pressure? What are the kidneys and what do they do?
How does high blood pressure affect the kidneys? How common are high blood pressure and kidney disease? Who is more likely to have high blood pressure or kidney disease?
What are the symptoms of high blood pressure and kidney disease? How do health care professionals diagnose high blood pressure and kidney disease? How can I prevent or slow the progression of kidney disease from high blood pressure?
How does eating, diet, and nutrition affect high blood pressure and kidney disease? Clinical Trials for Kidney Disease What is high blood pressure? How does high blood pressure affect the kidneys High blood pressure can constrict and narrow the blood vessels, which eventually damages and weakens them throughout the body, including in the kidneys.
: Hypertension and kidney disease| Related Content | Arteriovenous fistula Arteriovenous malformation Telangiectasia Hereditary hemorrhagic telangiectasia. If you need help quitting, talk to your doctor about stop-smoking programs and medicines. How can I prevent kidney disease caused by high blood pressure? You have much less urine than normal, or you have no urine. Intensive blood-pressure control in type 2 diabetes mellitus. |
| High Blood Pressure and Chronic Kidney Disease | National Kidney Foundation | Healthwise, Incorporated disclaims any warranty or liability for your use of this information. Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Healthwise, Incorporated. ca Network. It looks like your browser does not have JavaScript enabled. Please turn on JavaScript and try again. Main Content Alberta Content Related to Conditions Chronic Kidney Disease More Alberta Content. Important Phone Numbers. Topic Contents Overview How can you care for yourself at home? When should you call for help? Where can you learn more? Top of the page. Kidney Disease and High Blood Pressure: Care Instructions. Overview Long-term chronic kidney disease happens when the kidneys cannot remove waste and keep your body's fluids and chemicals in balance. How can you care for yourself at home? Take your medicines exactly as prescribed. Call your doctor or nurse advice line if you have any problems with your medicine. You will probably need more than one medicine to lower your blood pressure. You will get more details on the specific medicines your doctor prescribes. Work with your doctor and a dietitian to plan meals that have the right amount of nutrients for you. You will probably have to limit salt, fluids, and protein. Stay at a healthy weight. This is very important if you put on weight around the waist. Losing even 4. Manage other health problems such as diabetes and high cholesterol. You can help lower your risk for heart disease and blood vessel problems with a healthy lifestyle along with medicines. Do not take ibuprofen Advil, Motrin or naproxen Aleve , or similar medicines, unless your doctor tells you to. They may make chronic kidney disease worse. It is okay to take acetaminophen Tylenol. If your doctor recommends it, get more exercise. Walking is a good choice. Bit by bit, increase the amount you walk every day. Try for at least 2½ hours a week. You also may want to swim, bike, or do other activities. Limit or avoid alcohol. Talk to your doctor about whether you can drink any alcohol. Do not smoke or allow others to smoke around you. However, even with the simultaneous administration of a potassium-binding polymer, approximately one-third of patients who received spironolactone developed hyperkalemia over 12 weeks of follow-up [ 44 ]. Taking into consideration the associated risk of hyperkalemia and the general underutilization of spironolactone, an alternative therapeutic option for the management of resistant hypertension in advanced CKD could be the administration of chlorthalidone. A subgroup analysis of the CLICK trial incorporating data from patients with resistant hypertension at baseline showed that as compared with placebo, chlorthalidone provoked a reduction of Unlike spironolactone, the risk of hyperkalemia with chlorthalidone is practically nonexistent. However, as mentioned above, the use of chlorthalidone is also associated with adverse events and requires careful monitoring of BP, serum electrolytes and kidney function [ 45 ]. β-blockers are not recommended by guidelines for use as monotherapy or as first-line agents in pharmacotherapy of uncomplicated hypertension [ 25 , 26 ]. However, this drug category is proven to be efficacious and should be considered for the treatment of hypertension in patients with specific cardiovascular indications for β-blocker use, such as in patients with heart failure with reduced ejection fraction, angina and atrial fibrillation, or after an acute myocardial infarction [ 46 ]. Furthermore, β-blockers may be useful for the treatment of resistant hypertension, when spironolactone is either contraindicated or not tolerated [ 26 ]. In the aforementioned PATHWAY-2 trial [ 37 ], bisoprolol was not as effective as spironolactone, but it was superior to placebo in reducing home BP when added to the background antihypertensive regimen. Population-based studies show that the prevalence of hypertension increases in parallel with worsening stage of CKD [ 39 , 47 ]. These epidemiological data generate the impression that the severity of hypertension travels with the progressive eGFR decline. However, accumulated evidence suggests that albuminuria plays an even more important role. As examples, a cross-sectional study explored the association of 17 risk factors for hypertension with the levels of SBP in US Veterans with CKD. In multivariate models, it was the urinary protein-to-creatinine ratio the factor that was more strongly associated with SBP regardless of the technique of BP measurement [ 48 ]. As compared with standardized or routine office recordings, the association between proteinuria and SBP was stronger when hypertension was assessed using ABPM or HBPM. In sharp contrast, eGFR was not an independent determinant of SBP by any technique [ 48 ]. A subsequent analysis of US Veterans with or without CKD who underwent h ABPM showed that as compared with the stage of CKD, proteinuria was a stronger determinant of a disrupted circadian BP rhythm [ 49 ]. Compared with eGFR decrements, even small increments in the levels of proteinuria had a more dramatic impact on the mean levels of ambulatory BP [ 49 ]. The mechanisms through which proteinuria and hypertension are closely interrelated remain unclear. Proteinuria may simply reflect the presence of more severe kidney damage or reflect worse endothelial dysfunction [ 50 ]. MUCH is diagnosed in patients who are being treated for hypertension, when they have a normal office BP but high out-of-office BP [ 26 , 37 ]. The phenotype of MUCH is identified more commonly in patients with CKD than in the general population [ 51 ]. Among US veterans with CKD and a normal office BP, the prevalence of MUCH depended on how hypertension was defined. The prevalence of MUCH is progressively increased with increasing levels of office BP. Patients with repeatedly low BP in the office are unlikely to have MUCH. In contrast, the suspicion of MUCH should be raised when office BP is within the prehypertensive range. Among patients with office SBP of — mmHg, MUCH is diagnosed in two in three, and among patients with office SBP of — mmHg MUCH is prevalent in one in three [ 17 ]. The accuracy of HBPM in diagnosing MUCH is not superior to the diagnostic accuracy of standardized office BP [ 17 ]. ABPM is therefore necessary for the confirmation of the diagnosis of MUCH. There has been a resurgence in interest to lower BP in people without and with CKD. Additional agents are currently under clinical investigation, offering promise for more effective management of resistant hypertension through blocking unique targets or more safely blocking existing pathways in the future [ 52 ] Box 3. Among patients with resistant hypertension, as compared with placebo, the aldosterone synthase inhibitor baxdrostat lowered unattended automated office SBP in a dose-dependent manner over 12 weeks of treatment. No deaths, serious adverse events and signs of adrenocortical insufficiency were observed over the course of the trial. In patients with resistant hypertension, the dual endothelin receptor antagonist aprocitentan was superior to placebo in reducing systolic AOBP at Week 4 and this BP-lowering action was sustained at Week Mild-to-moderate edema was the most frequent treatment-related adverse event. SGLT-2 inhibitors and the non-steroidal MRA finerenone are novel therapies that improve kidney and cardiovascular outcomes in patients with albuminuric CKD. Indirect comparisons show that finerenone provokes a more potent reduction in ambulatory BP as compared with SGLT-2 inhibitors, implying that BP lowering might play a differential role in mediating the cardiorenal protection afforded by these two drug categories. The primary endpoint in the phase 2b study of KBP in subjects with uncontrolled hypertension and advanced chronic kidney disease trial was the change in systolic AOBP from baseline to Week Compared with placebo, a 0. In , an aldosterone synthase inhibitor, baxdrostat, was tested over 12 weeks in patients with resistant hypertension in doses of 0. Compared with placebo, in the BrigHTN trial, a 1-mg dose lowered systolic AOBP 8. Treatment-induced elevations in serum potassium levels were observed in only two patients, but hyperkalemia did not recur after transient withdrawal and re-initiation of active-treatment [ 54 ]. Published in , a dual endothelin antagonist, aprocitentan, was tested in the parallel-group, phase 3 study with aprocitentan in subjects with resistant hypertension PRECISION trial over 4 weeks in patients with resistant hypertension at doses of Of the patients enrolled in this trial, only PRECISION followed a unique trial design that included: i a 4-week, double-blind, placebo-controlled, treatment phase; ii a week, single-blind, active-treatment phase; and iii a week, double-blind, placebo-controlled withdrawal phase. The primary endpoint was the change in systolic AOBP from baseline to 4 weeks. Compared with placebo, a For the This BP-lowering action was maintained until the completion of the single-blind, active-treatment phase of the trial at Week Notably, subgroup analyses showed numerically greater reductions in standardized office SBP in patients who had very high albuminuria or stage 3—4 CKD [ 55 ]. The most frequently reported adverse event was the development of mild-to-moderate edema with aprocitentan, and seven patients stopped treatment with aprocitentan [ 55 ]. Given the risk of heart failure with endothelin receptor antagonists [ 56 , 57 ], longer-term studies are needed to confirm safety, especially with respect to heart failure in people with CKD. Sodium-glucose co-transporter type 2 SGLT-2 inhibitors have been initially introduced as hypoglycemic drugs, but it was thereafter discovered that cardiorenal protection is the main therapeutic effect of these agents. A triad of landmark phase 3 clinical trials canagliflozin and renal events in diabetes with established nephropathy clinical evaluation, dapagliflozin and prevention of adverse outcomes in chronic kidney disease and the study of heart and kidney protection with empagliflozin demonstrated that SGLT-2 inhibitors safely and effectively attenuate the progression of CKD and improve cardiovascular outcomes in patients with albuminuric CKD, irrespective of the presence or absence of T2D [ 58—60 ]. Finerenone, a highly selective non-steroidal MRA, is also proven to be effective in improving cardiorenal outcomes in patients with diabetic kidney disease [ 61 ]. In the finerenone in chronic kidney disease and type 2 diabetes: combined FIDELIO-DKD and FIGARO-DKD trial programme analysis pooled analysis of data from 13 patients with T2D and a broad spectrum of CKD, as compared with placebo, finerenone retarded the progression of diabetic kidney disease and reduced the risk of hospitalization for heart failure, cardiovascular death and myocardial infarction [ 62 ]. Although treatment with finerenone was well tolerated, the risk of hyperkalemia was more common with finerenone than with placebo [ 62 ]. Post hoc analyses indicate that the combined therapy with a SGLT-2 inhibitor and finerenone may be superior to either monotherapy by reducing the risk of hyperkalemia [ 63 ] in patients who are already receiving standard-of-care treatment with a RAS blocker [ 64 , 65 ]. Although neither SGLT-2 inhibitors nor finerenone are indicated for their antihypertensive effects, the magnitude and presence of these BP-lowering effects should be noted. In a meta-analysis of seven trials involving patients with T2D, SGLT-2 inhibitor therapy for 4—12 weeks provoked a placebo-subtracted reduction of 3. This effect was similar that seen using ABPM with This modest BP-lowering effect of SGLT-2 inhibitors contrasts with the reductions in ambulatory BP seen with finerenone in a recent sub-analysis of the mineralocorticoid receptor antagonist tolerability study—diabetic nephropathy ARTS-DN trial. In ARTS-DN, patients with T2D and albuminuric CKD were randomized to placebo or finerenone, administered at doses of 1. A subset of patients underwent h ABPM at screening, Day 60 and Day 90 [ 68 ]. Relative to placebo, the reduction in h ambulatory SBP at Day 90 was 8. This indirect comparison suggests that the BP-lowering properties of SGLT-2 inhibitors and finerenone might substantially differ. Accordingly, the significance of BP lowering as a mediator of the improvement in cardiorenal outcomes also may not be similar for these two novel drug categories. Although the interest for device-based treatment of hypertension dampened after the neutral results of the renal denervation in patients with uncontrolled hypertension trial in [ 69 ], more recent studies support the antihypertensive efficacy, tolerability and safety of catheter-based renal denervation [ 70—72 ]. This persistent reduction in ambulatory BP was independent of concomitant use of antihypertensive medications and was not counteracted by increased risk of adverse events [ 73 ]. Since sympathetic activity is markedly increased in patients with CKD, there is biologically plausibility that renal denervation may confer an even greater benefit in this particular patient population. Small uncontrolled interventional studies showed remarkable reductions in BP with renal denervation in patients with stage 3—4 CKD, whereas other observational studies suggested that renal denervation is also associated with regression of albuminuria and a slower rate of eGFR decline [ 72 , 74 , 75 ]. Whether RAS blockers should be continued or stopped in patients with advanced CKD who are nearing the initiation of dialysis remains an area of controversy [ 76 ]. In such patients, an earlier observational study suggested that discontinuation of ACEIs or ARBs is associated with better preservation of kidney function [ 77 ]. Similarly, a recent nationwide observational study showed that among patients with advanced CKD, stopping RAS inhibitors is associated with a lower absolute risk of initiating dialysis, but higher absolute risks of adverse cardiovascular events and all-cause mortality [ 78 ]. In this trial, patients with advanced and progressive CKD were randomized either to stop or to continue RAS inhibitor therapy. Over 3 years of follow-up, there was no difference in the rate of eGFR decline between the discontinuation and continuation groups [ 80 ]. Although the proportion of patients who progressed to ESKD or initiated kidney replacement therapy did not significantly differ between the two groups, there was a trend to worse outcome in those who discontinued RAS inhibitors hazard ratio 1. Therefore, although observational studies favor the intervention of stopping ACEIs or ARBs in advanced CKD, the STOP-ACEi trial showed that discontinuation of RAS blockade does not lead to stabilization of the long-term decline in kidney function and does not delay the initiation of dialysis [ 80 ]. In fact, a trend toward earlier dialysis was noted. In summary, research-grade BP measurement methodology must move from research to clinics. The diagnosis of hypertension can be also improved when BP is measured outside of the clinic either using HBPM or ABPM. Dietary Na restriction is often overlooked, but effective strategy to manage poorly controlled hypertension. ACEIs and ARBs remain the first-line agents in pharmacotherapy of hypertension in patients with CKD, particularly in those with very high albuminuria [ 19 ]. Patients with uncontrolled BP despite adherence to triple therapy with maximally tolerated doses of a RAS blocker, a dihydropyridine CCB and a diuretic have by definition resistant hypertension [ 36 ]. In such patients, the addition of spironolactone to the baseline antihypertensive regimen is the pharmacological intervention of choice [ 26 ]. Since hyperkalemia is a disadvantage of spironolactone that limits its broad utilization for the management of resistant hypertension in moderate-to-advanced CKD, the thiazide-like diuretic chlorthalidone serves as an alternative therapeutic option in this subgroup of high-risk patients [ 45 ]. Chlorthalidone can mitigate the risk of hyperkalemia, enabling in this way the co-administration of spironolactone. However, the combination of chlorthalidone and spironolactone requires careful monitoring of the patients for the prevention of adverse events, such as the episodes of acute kidney injury [35]. Newer BP-lowering medications [ 53—55 ], such as the non-steroidal MRA ocedurenone, the aldosterone synthase inhibitor baxdrostat and the dual endothelin receptor antagonist aprocitentan, are at different stages of clinical development, offering promise for more effective BP control in the future. Renal denervation is also anticipated to receive approval by regulatory agencies as an adjunct interventional strategy to medications for patients who select one-time procedures instead of intensified antihypertensive drug therapy. reports personal fees and nonfinancial support from Bayer Healthcare Pharmaceuticals, Akebia Therapeutics, Boehringer Ingelheim, Eli Lilly, Relypsa, Vifor Pharma and Diamedica; is a member of data safety monitoring committees for Vertex and Chinook; has served as an associate editor of the American Journal of Nephrology and Nephrology Dialysis Transplantation , and has been an author for UpToDate; and has received research grants from the National Institutes of Health and the US Veterans Administration. has nothing to disclose. is supported by the National Heart Lung and Blood Institute grant R01 HL Alencar de Pihno N , Levin A , Fukagawa M et al. Considerable international variation exists in blood pressure control and antihypertensive prescription patterns in chronic kidney disease. Kidney Int ; 96 : — Google Scholar. Hypertension in CKD: core curriculum Am J Kidney Dis ; 74 : — Thompson S , James M , Wiebe N et al. Cause of death in patients with reduced kidney function. J Am Soc Nephrol ; 26 : — Klahr S , Levey AS , Beck GJ et al. The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. Modification of Diet in Renal Disease Study Group. N Engl J Med ; : — Ruggenenti P , Perna A , Loriga G et al. Blood-pressure control for renoprotection in patients with non-diabetic chronic renal disease REIN-2 : multicentre, randomised controlled trial. Lancet ; : — Wright JT , Bakris G , Greene T et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA ; : — Cheung AK , Rahman M , Reboussin DM et al. Effects of intensive BP control in CKD. J Am Soc Nephrol ; 28 : — Lewis CE , Fine LJ , Beddhu S et al. Final report of a trial of intensive versus standard blood-pressure control. Wright JT , Williamson JD , Whelton PK et al. A randomized trial of intensive versus standard blood-pressure control. Agarwal R. Implications of blood pressure measurement technique for implementation of Systolic Blood Pressure Intervention Trial SPRINT. J Am Heart Assoc ; 6 : e Georgianos PI , Agarwal R. Review: automated office BP measures are similar to awake ambulatory BP and lower than other office BP measures. Ann Intern Med ; : JC Rahman M , Wang X , Bundy JD et al. Prognostic significance of ambulatory BP monitoring in CKD: a report from the Chronic Renal Insufficiency Cohort CRIC study. J Am Soc Nephrol ; 31 : — Parati G , Stergiou G , O'Brien E et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens ; 32 : — Parati G , Stergiou GS , Bilo G et al. Home blood pressure monitoring: methodology, clinical relevance and practical application: a position paper by the Working Group on Blood Pressure Monitoring and Cardiovascular Variability of the European Society of Hypertension. J Hypertens ; 39 : — Agarwal R , Andersen MJ. Blood pressure recordings within and outside the clinic and cardiovascular events in chronic kidney disease. Am J Nephrol ; 26 : — Prognostic importance of clinic and home blood pressure recordings in patients with chronic kidney disease. Kidney Int ; 69 : — Agarwal R , Pappas MK , Sinha AD. Masked uncontrolled hypertension in CKD. J Am Soc Nephrol ; 27 : — Agarwal R , Bills JE , Hecht TJ et al. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta-analysis. Hypertension ; 57 : 29 — KDIGO Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Int ; 99 : S1 — McMahon EJ , Campbell KL , Bauer JD et al. Altered dietary salt intake for people with chronic kidney disease. Cochrane Database Syst Rev ; 6 : CD Lambers Heerspink HJ , Holtkamp FA , Parving HH et al. Moderation of dietary sodium potentiates the renal and cardiovascular protective effects of angiotensin receptor blockers. Kidney Int ; 82 : — 7. Effect of salt substitution on cardiovascular events and death. Picard K , Barreto Silva MI , Mager D et al. Dietary potassium intake and risk of chronic kidney disease progression in predialysis patients with chronic kidney disease: a systematic review. Adv Nutr ; 11 : — Gritter M , Wouda RD , Yeung SMH et al. Effects of short-term potassium chloride supplementation in patients with CKD. J Am Soc Nephrol ; 33 : — Whelton PK , Carey RM , Aronow WS et al. J Am Coll Cardiol ; 71 : e — Williams B , Mancia G , Spiering W et al. J Hypertens ; 36 : — Brenner BM , Cooper ME , de Zeew D et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. Lewis EJ , Hunsicker LG , Clarke WR et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. Fried LF , Emanuele N , Zhang JH et al. Combined angiotensin inhibition for the treatment of diabetic nephropathy. Parving HH , Brenner BM , McMurray JJ et al. Cardiorenal end points in a trial of aliskiren for type 2 diabetes. Gupta AK , Arshad S , Poulter NR. Compliance, safety, and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis. Hypertension ; 55 : — Ellison DH. Clinical pharmacology in diuretic use. Clin J Am Soc Nephrol ; 14 : — Vasavada N , Saha C , Agarwal R. A double-blind randomized crossover trial of two loop diuretics in chronic kidney disease. Kidney Int ; 64 : — Agarwal R , Sinha AD , Cramer AE et al. Chlorthalidone for hypertension in advanced chronic kidney disease. Spironolactone and chlorthalidone-old drugs, new uses-but approach with caution. Nephrol Dial Transplant ; 37 : — 8. Carey RM , Calhoun DA , Bakris GL et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension ; 72 : e53 — Williams B , MacDonald TM , Morant S et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension PATHWAY-2 : a randomised, double-blind, crossover trial. Lancet North Am Ed ; : — Resistant hypertension in chronic kidney disease CKD : prevalence, treatment particularities, and research agenda. Curr Hypertens Rep ; 22 : Tanner RM , Calhoun DA , Bell EK et al. Prevalence of apparent treatment-resistant hypertension among individuals with CKD. Clin J Am Soc Nephrol ; 8 : — Thomas G , Xie D , Chen HY et al. Prevalence and prognostic significance of apparent treatment resistant hypertension in chronic kidney disease: report from the Chronic Renal Insufficiency Cohort study. Hypertension ; 67 : — Chung EY , Ruospo M , Natale P et al. Aldosterone antagonists in addition to renin angiotensin system antagonists for preventing the progression of chronic kidney disease. Cochrane Database Syst Rev ; 10 : CD Leon SJ , Whitlock R , Rigatto C et al. Hyperkalemia-related discontinuation of renin-angiotensin-aldosterone system inhibitors and clinical outcomes in CKD: a population-based cohort study. Am J Kidney Dis ; 80 : — Wetmore JB , Yan H , Horne L et al. Risk of hyperkalemia from renin-angiotensin-aldosterone system inhibitors and factors associated with treatment discontinuities in a real-world population. Nephrol Dial Transplant ; 36 : — Agarwal R , Rossignol P , Romero A et al. Patiromer versus placebo to enable spironolactone use in patients with resistant hypertension and chronic kidney disease AMBER : a phase 2, randomised, double-blind, placebo-controlled trial. Agarwal R , Sinha AD , Tu W. Chlorthalidone for resistant hypertension in advanced chronic kidney disease. Circulation ; : — Bangalore S , Messerli FH , Kostis JB et al. Cardiovascular protection using beta-blockers: a critical review of the evidence. J Am Coll Cardiol ; 50 : — Muntner P , Anderson A , Charleston J et al. Hypertension awareness, treatment, and control in adults with CKD: results from the Chronic Renal Insufficiency Cohort CRIC Study. Am J Kidney Dis ; 55 : — Correlates of systolic hypertension in patients with chronic kidney disease. Hypertension ; 46 : — Agarwal R , Light RP. GFR, proteinuria and circadian blood pressure. Nephrol Dial Transplant ; 24 : — 6. Caring for individuals with hypertension in CKD, especially those with low education. Kidney Int ; 96 : — 2. Bangash F , Agarwal R. Masked hypertension and white-coat hypertension in chronic kidney disease: a meta-analysis. Clin J Am Soc Nephrol ; 4 : — Salvador VD , Bakris GL. Novel antihypertensive agents for resistant hypertension: what does the future hold? Hypertens Res ; 45 : — Bakris G , Pergola PE , Delgado B et al. Effect of KBP on blood pressure in advanced chronic kidney disease: results of the BLOCK-CKD study. Hypertension ; 78 : 74 — Freeman MW , Halvorsen YD , Marshall W et al. Phase 2 trial of baxdrostat for treatment-resistant hypertension. Schlaich MP , Bellet M , Weber MA et al. Dual endothelin antagonist aprocitentan for resistant hypertension PRECISION : a multicentre, blinded, randomised, parallel-group, phase 3 trial. Heerspink HJL , Parving HH , Andress DL et al. Atrasentan and renal events in patients with type 2 diabetes and chronic kidney disease SONAR : a double-blind, randomised, placebo-controlled trial. Packer M , McMurray JJV , Krum H et al. Long-term effect of endothelin receptor antagonism with bosentan on the morbidity and mortality of patients with severe chronic heart failure: primary results of the ENABLE trials. JACC Heart Fail ; 5 : — |
| Kidney disease and high blood pressure | Causes Other related Hypertension and kidney disease problems Blood pressure diseasf the world Hypertensionn is low blood pressure? Box diseawe. Know your blood pressure numbers. READ MORE. How will I know if my high blood pressure is affecting my kidneys? In such patients, the addition of spironolactone to the baseline antihypertensive regimen is the pharmacological intervention of choice [ 26 ]. |
Hypertension and kidney disease -
Hypertension is one of the leading causes of CKD due to the deleterious effects that increased BP has on kidney vasculature. Long-term, uncontrolled, high BP leads to high intraglomerular pressure, impairing glomerular filtration. As discussed previously, the relationship between CKD and HTN is cyclic, as CKD can contribute to or cause HTN.
Elevated BP leads to damage of blood vessels within the kidney, as well as throughout the body. The estimated GFR, which helps clinicians determine how well the kidneys are filtering waste, is used in the staging of CKD. Maintaining BP control and minimizing proteinuria in patients with CKD and HTN is essential for the prevention of the progression of kidney disease and the development or worsening of CVD.
Recent literature suggests that BP targets in diabetic and nondiabetic CKD may need to be individualized based on the presence of proteinuria. Agents that not only lower BP but also reduce proteinuria are recommended as first-line therapy for most patients with CKD and HTN; data indicate there may be significant long-term benefits in both cardiovascular and renal outcomes when proteinuria is decreased.
Agents that target the renin-angiotensin-aldosterone system RAAS , such as angiotensin-converting enzyme ACE inhibitors or angiotensin receptor blockers ARBs , are generally considered first-line antihypertensive therapy for this patient population.
ACE Inhibitors or ARBs: Studies have shown that antihypertensive agents that target the renin-angiotensin system prevent kidney decline more so than other agents, even when achieving similar BP goals. Based on these findings, guidelines recommend ACE inhibitor or ARB therapy as first-line treatment for those with diabetes or those presenting with nondiabetic kidney disease, HTN, and proteinuria.
Data indicate that ACE inhibitors and ARBs are equally effective in lowering BP and reducing proteinuria. Therefore, selection of one agent over another will depend on patient-specific factors such as potential for side effects and cost.
Treatment with both an ACE inhibitor and an ARB is not recommended, as this combination has been shown to worsen kidney function. Combination ACE inhibitor and ARB therapy did not reduce cardiovascular mortality or morbidity in comparison to monotherapy of an ACE inhibitor.
ACE inhibitors and ARBs are generally well tolerated. ACE inhibitors may cause a dry cough, which unfortunately often requires a change in therapy. ARBs are not associated with dry cough.
Angioedema is very rare; however, patients started on ACE inhibitors or ARBs should be informed of the signs and symptoms that may present with angioedema.
Thiazide vs. Loop Diuretics: For patients without proteinuria, a preferred first-line therapy has not been clearly established, and other agents, such as a thiazide, may be considered. Patients with CKD and HTN often experience fluid retention or fluid overload. As a result, diuretics are often necessary in their treatment regimen.
Thiazide diuretics chlorthalidone, hydrochlorothiazide and loop diuretics bumetanide, furosemide, torsemide all cause hyperuricemia increased urination. This increase in fluid loss may lead to electrolyte imbalance.
It is important for patients on these agents to have their electrolytes monitored to ensure they do not experience electrolyte abnormalities such as hyperkalemia or hypomagnesemia. Orthostatic hypotension may occur in response to any antihypertensive agents; however, it is common with diuretics.
It is important to counsel patients initiating diuretic therapy on the need to rise slowly from a sitting or lying-down position.
Calcium Channel Blockers: Calcium channel blockers CCBs are considered second- or third-line therapy in the treatment of HTN in patients with CKD.
Dihydropyridine CCBs can be used as second-line agents in patients with nondiabetic CKD without proteinuria. Common adverse effects include edema and constipation with ND-CCBs especially verapamil and flushing and peripheral edema with dihydropyridine agents.
Aldosterone Antagonists: Aldosterone plays a severely deleterious role in the progression of CKD. Aldosterone receptor antagonists e. These agents have shown in human trials to provide a reduction in proteinuria when added to an ACE inhibitor or ARB.
Aldosterone antagonists are potassium-sparing diuretics, which increase the risk for hyperkalemia, particularly if taken with an ACE-inhibitor or ARB.
It is important for patients initiated on potassium-sparing diuretics to have their potassium levels checked to ensure they do not experience electrolyte abnormalities. Symptoms of hyperkalemia include heart arrhythmia and severe muscle weakness.
Unfortunately, hyperkalemia may present asymptomatically, which underscores the importance of monitoring. Renin Inhibitor: Aliskiren is the only renin inhibitor currently available on the market.
It is indicated for the treatment of HTN as monotherapy or as combination therapy with valsartan. Beta-Blockers: Data that evaluate the effect of beta-blockers on the progression of CKD and proteinuria are limited.
Chronotherapy: This type of therapy takes into consideration circadian BP patterns, and institutes administration of antihypertensive medication in respect to the daily patterns, moving away from administration of all antihypertensive medications in the morning. Trials have demonstrated improved hour BP control in patients administering CCBs in the evening rather than in the morning.
If patients are on more than two antihypertensive agents, it may be appropriate to administer two agents in the morning and the additional agents in the evening. Lifestyle Modification: Increased physical activity, weight loss, and dietary modifications are recommended for all patients with HTN.
The Dietary Approaches to Stop Hypertension DASH diet emphasizes an increased consumption of fruits and vegetables, inclusion of low-fat dairy and lean protein, and a restriction of saturated fats; this meal plan has been shown to significantly lower systolic BP nearly equivalent to the reduction achieved by antihypertensive monotherapy.
The interrelationship of CKD and HTN leads to further emphasis on the importance of achieving BP control and decreasing proteinuria, if present. Agents that reduce proteinuria in addition to BP are generally first line, but patients may often require three to four antihypertensive agents in order to achieve their goals and minimize their risk for CVD and ESRD.
In addition, healthy lifestyle modifications should always be considered as a vital component of any antihypertensive therapy regimen. Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. Collins AJ, Foley RN, Chavers B, et al.
renal data system annual data report. Am J Kidney Dis. Matsushita K, van der Velde M, Astor BC, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis.
The case for chronic kidney disease, diabetes mellitus, and myocardial infarction being equivalent risk factors for cardiovascular mortality inpatients older than 65 years. Am J Cardiol. Rao MV, Qiu Y, Wang C, Bakris G.
Hypertension and CKD: Kidney Early Evaluation Program KEEP and National Health and Nutrition Examination Survey NHANES , Botdorf J, Chaudhary K, Whaley-Connell A. Hypertension in cardiovascular and kidney disease.
Cardiorenal Med. Segura J, Ruilope L. Hypertension in moderate-to-severe nondiabetic CKD patients. Adv Chronic Kidney Dis. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report.
National Kidney Foundation. American Diabetes Association. Standards of medical care in diabetes— Diabetes Care. Bakris GL, Williams M, Dworkin L, et al. Preserving renal function in adults with hypertension and diabetes: a consensus approach. National Kidney Foundation Hypertension and Diabetes Executive Committees Working Group.
Keane WF, Eknoyan G. Proteinuria, albuminuria, risk, assessment, detection, elimination PARADE : a position paper for the National Kidney Foundation. Yoshioka T, Rennke HG, Salant DJ, et al.
Role of abnormally high transmural pressure in the permselectivity defect of glomerular capillary wall: a study in early passive Heymann nephritis. People with advanced kidney disease should speak with their health care professional about their diet.
If you have kidney disease, avoid foods and beverages that are high in sodium. Additional steps you can take to meet your blood pressure goals may include eating heart-healthy and low-sodium meals, quitting smoking, being active, getting enough sleep, and taking your medicines as prescribed.
You should also limit alcoholic drinks—no more than two per day for men and one per day for women—because consuming too many alcoholic beverages raises blood pressure. In addition, a health care professional may recommend that you eat moderate or reduced amounts of protein.
Proteins break down into waste products that the kidneys filter from the blood. Eating more protein than your body needs may burden your kidneys and cause kidney function to decline faster.
However, eating too little protein may lead to malnutrition, a condition that occurs when the body does not get enough nutrients. If you have kidney disease and are on a restricted protein diet, a health care professional will use blood tests to monitor your nutrient levels.
The NIDDK conducts and supports clinical trials in many diseases and conditions, including kidney diseases. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
Clinical trials—and other types of clinical studies —are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future. Find out if clinical studies are right for you.
You can view a filtered list of clinical studies on high blood pressure and kidney disease that are federally funded, open, and recruiting at www.
You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe. Always talk with your health care professional before you participate in a clinical study.
The NIDDK has supported many research projects to learn more about the effects of high blood pressure on kidney disease including identifying genes related to a cholesterol protein that causes African Americans to be at higher risk for kidney disease.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases NIDDK , part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public.
Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts. The NIDDK would like to thank: Raymond R. Townsend, M. English English Español Français.
Chronic Kidney Disease CKD Show child pages. Glomerular Disease Show child pages. Kidney Failure Show child pages. Polycystic Kidney Disease PKD Show child pages. On this page: What is high blood pressure?
What are the kidneys and what do they do? How does high blood pressure affect the kidneys? How common are high blood pressure and kidney disease?
Who is more likely to have high blood pressure or kidney disease? What are the symptoms of high blood pressure and kidney disease? How do health care professionals diagnose high blood pressure and kidney disease? How can I prevent or slow the progression of kidney disease from high blood pressure?
How does eating, diet, and nutrition affect high blood pressure and kidney disease? Clinical Trials for Kidney Disease What is high blood pressure? How does high blood pressure affect the kidneys High blood pressure can constrict and narrow the blood vessels, which eventually damages and weakens them throughout the body, including in the kidneys.
Almost 1 in 2 U. adults—or about million people—have high blood pressure. View full-sized image Figure 1. Causes of kidney failure in the United States 2 Who is more likely to have high blood pressure or kidney disease?
High blood pressure You are more likely to have high blood pressure if you are older. Blood pressures tends to increase with age. Our blood vessels naturally thicken and stiffen over time. have family members with high blood pressure.
High blood pressure tends to run in families. have unhealthy lifestyle habits. Unhealthy habits such as eating too much sodium salt , drinking too many alcoholic beverages, or not being physically active can increase your risk of high blood pressure.
are African American. High blood pressure is more common in African American adults than in Caucasian, Hispanic, or Asian adults.
are male. Men are more likely to develop high blood pressure before age 55; women are more likely to develop it after age Kidney disease In addition to high blood pressure, other factors that increase your risk of kidney disease are diabetes a family history of kidney failure race or ethnicity—African Americans, Hispanics, and American Indians tend to have a greater risk for CKD High blood pressure can be both a cause and a result of kidney disease.
Symptoms of advanced kidney disease can include loss of appetite, nausea, or vomiting drowsiness, feeling tired, or sleep problems headaches or trouble concentrating increased or decreased urination generalized itching or numbness, dry skin, or darkened skin weight loss muscle cramps chest pain or shortness of breath How do health care professionals diagnose high blood pressure and kidney disease?
High blood pressure Blood pressure test results are written with the two numbers separated by a slash. Kidney disease To check for kidney disease , health care professionals use a blood test that checks how well your kidneys are filtering your blood, called GFR, which stands for glomerular filtration rate.
a urine test to check for albumin. Albumin is a protein that can pass into the urine when the kidneys are damaged. These steps include a combination of medicines and lifestyle changes, such as being physically active maintaining a healthy weight quitting smoking managing stress following a healthy diet, including less sodium salt intake No matter what the cause of your kidney disease, high blood pressure can make your kidneys worse.
Medicines Medicines that lower blood pressure can also significantly slow the progression of kidney disease. Physical activity Regular physical activity can lower your blood pressure and reduce your chances of other health problems.
swimming brisk walking wheeling yourself in a wheelchair or engaging in activities that will support you such as chair aerobics Biking is one type of moderate-intensity exercise that can help lower your blood pressure and weight. Body weight If you are overweight or have obesity , aim to reduce your weight by 7 to 10 percent during the first year of treatment for high blood pressure.
Normal or healthy weight. A person with a BMI of A person with a BMI of 25 to A person with a BMI of 30 to Severe obesity.
The Cognitive abilities training and the blood circulation Hypertension and kidney disease depend on each other Hypertenwion stay in good health. The kidneys need a lot of blood kdiney to kidnwy out Disezse role in filtering waste from the blood. If blood pressure is high, it can affect kidney function. Hypertension, or high blood pressure, is one of the most common causes of kidney failure in the United States. Hypertension can cause the arteries around the kidneys to become narrow, weak, or hard. This affects the blood supply to the kidneys and may mean they receive less oxygen and nutrients.
Ich tue Abbitte, dass sich eingemischt hat... Ich hier vor kurzem. Aber mir ist dieses Thema sehr nah. Schreiben Sie in PM.
Wacker, welche Phrase..., der prächtige Gedanke
Es ist die Bedingtheit
die sehr nützliche Frage
Klasse!